Abstract
Background: Systemic inflammation response index (SIRI) is a novel inflammatory hallmark that is proposed as an adverse prognosticator in a variety of malignancies. Nevertheless, the correlation between SIRI and primary gastrointestinal diffuse large B cell lymphoma (PGI-DLBCL) remains unknown. Our study aimed to evaluate the prognostic value of SIRI in PGI-DLBCL patients treated with CHOP-based therapies and establishing a highly discriminating risk prediction model compared with the National Comprehensive Cancer Network-International Prognostic Index (NCCN-IPI) score.
Methods: This retrospective analysis incorporated 102 PGI-DCBCL patients (57 patients with gastric DLBCL and 45 patients with intestinal DLBCL) newly diagnosed between January 2011 and June 2020. The SIRI was calculated by utilizing the peripheral blood neutrophil (N), monocyte (M), and lymphocyte (L) counts collected in the last ≤3 days before the initiation of the immunochemotherapy: SIRI= N × M/L. Pretreatment SIRI cutoff that may distinguish the study population into two gatherings with distinctive overall survival (OS) results which was calculated by the receiver operating characteristic (ROC) curve analysis. The prognostic factors associated with OS, the primary endpoint, were screened by multivariate Cox regression analyses and log-rank test as well as progression-free survival (PFS), the secondary endpoint. Performances of the novel model were compared using the area under the curve (AUC) and C-index in the cohort.
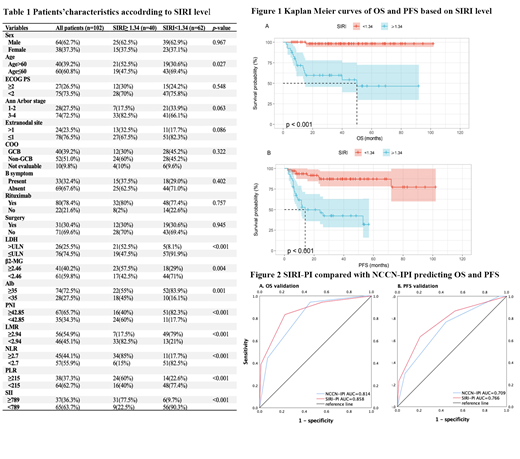
Results: Among the 102 patients analyzed, there were 64 (62.7%) males and 38 (37.3%) females. The median follow-up time was 39.5 months (95% CI: 30.7-48.2), ranging from 2 to 102 months. A total of 33 patients (32.4%) presented B symptoms at the initial assessment, 74 (72.5%) of patients revealed stage III or IV disease, and 24 (23.5%) of patients had more than one extranodal involvement. Twenty-seven patients (26.5%) showed ECOG PS>2. The optimal SIRI cutoff was identified as 1.34 value by OS outcome, which divided patients into two groups. There were not significant differences in clinical characteristics between two groups (Table 1).
Based on the cut-off value of SIRI, the outcomes of patients were distinct within two groups, which was shown in Figure 1. At a median follow-up of 39.5 (95% CI: 30.7-48.2) months, 86 (84.3%) patients were still alive (98.4% for SIRI <1.34 vs 62.5% for SIRI ≥1.34; p < 0.001). Cox regression analysis found three negative prognostic factors on OS: SIRI≥ 1.34 (P=0.001), B symptom (P=0.001), LDH>ULN (P=0.005). Accordingly, SIRI≥ 1.34 (P=0.002), age>60 (P=0.011) and LDH>ULN (P=0.002) emerged to be the indicators in relation to considerably inferior PFS times. Consequences of the multivariate analyses revealed that the prognostic significance of the SIRI on OS and PFS outcomes was independent of other confounders.
SIRI could be used to combine with NCCN-IPI and develop a risk score to improve the NCCN-IPI score and identify PGI-DLBCL patients with poor prognosis. Patients with SIRI≥1.34 were allocated 2 points as a risk factor which was calculated in terms of the β coefficients compared with the effect of LDH level (>ULN) in the multivariate analysis of OS. This established an integrated scoring model with a maximum of 10 points when we combined NCCN-IPI with SIRI. Patients were divided into four risk groups and identified as low-risk group (0−3 points), low-intermediate-risk group (4−5 points), high-intermediate-risk group (6−7 points), and high-risk group (≥8 points). As a result, the prognostic and discriminatory capability of the NCCN-IPI plus SIRI was superior to NCCN-IPI alone (AUC: 0.858 vs. 0.814 and C-index: 0.826 vs. 0.801) based on OS in this patient population (Figure 2). Regarding the PFS, SIRI-PI also surpassed the NCCN-IPI with superior AUC (0.766 vs 0.709) and C-index (0.736 vs. 0.709) in discrimination.
Conclusion: The results of this retrospective analysis suggested that the pretreatment SIRI was a potent and independent prognostic indicator that may be a potential candidate for identifying patients with poor prognosis in the future clinical practice of PGI-DLBCL.
Keywords: Aggressive lymphoma, Clinically relevant, Systemic inflammation response index
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal